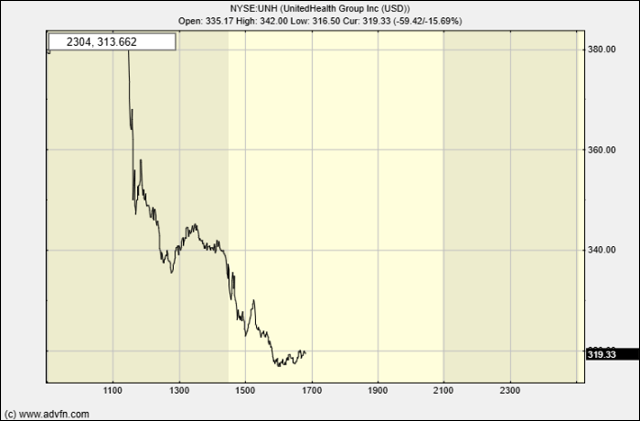
Shares of UnitedHealth Group (NYSE:UNH) fell sharply on Tuesday, dropping over 14% by mid-morning, after the healthcare giant paused its full-year guidance and announced a sudden leadership change. The stock has now lost 36% of its value since the start of the year.
The company revealed that CEO Andrew Witty is stepping down for personal reasons. In his place, UnitedHealth has reinstated former CEO Stephen Hemsley, who led the firm from 2006 to 2017. Hemsley will resume the CEO role immediately while also maintaining his position as Chairman of the Board. Witty will remain with the company temporarily in an advisory role.
Analysts at Bernstein described the leadership change as a “proactive move” in response to both strategic missteps and growing regulatory pressures. Witty’s tenure included several challenges, most notably the shooting death of Brian Thompson, the head of UnitedHealth’s insurance division, in late 2023. That incident led to heightened security for executives amid a rise in threats, and the company now faces a shareholder lawsuit claiming it failed to properly disclose the operational impact of Thompson’s death.
While UnitedHealth did not directly link Witty’s resignation to these events, the timing has raised questions.
Adding to the company’s woes, UnitedHealth also announced it is withdrawing its 2025 financial outlook. The company cited unexpectedly high medical costs, particularly from an influx of new Medicare Advantage enrollees. Health service usage among older adults has continued to grow, expanding into more areas of care than anticipated in the first quarter.
Despite these setbacks, UnitedHealth expressed confidence in its long-term trajectory and projected a return to growth in 2026.
The announcement follows UnitedHealth’s disappointing earnings report in April, which marked its first profit miss since 2008. Investors had hoped the firm would maintain its guidance on the back of strong demand for medical services. However, like many in the industry, UnitedHealth is contending with rising healthcare utilization, as more Medicare patients move forward with elective procedures that were delayed during the pandemic. Its Optum Health division, responsible for managing prescription plans under Medicare, has also faced cost pressures as patients require more care.